“I can’t bring you back”: Fentanyl’s deadly impact
Nalox Boxes, which contain the overdose reversal medication Naloxone, like these are available throughout the community. The closest one to Center Grove High School is at White River Public Library.
This story is part of a series of reports produced by Jack Forrest, Charlie LaRocca, Finn Nowacki, Tanu Kaur and Gourav Pany. This story was written by Charlie LaRocca.
“I can’t bring you back from fentanyl,” Resource Officer Jay Smallwood said. “You’ve chosen the kiss of death. I can’t wake you up.”
It was a blunt decree, maybe even one that seems obvious to most, but as the fentanyl crisis – and the greater American opioid crisis – continues to take more lives by the day, it is a necessary one.
In the case of fentanyl, a synthetic opioid up to 100 times more potent than morphine, the saying “a little goes a long way” rings with scary truth.
In March of this year, a student of Avon High school overdosed on fentanyl. Then just last month, another student passed — suspected to be a death of the same classification. As the issue compounds, awareness and education about the drug and its effects are essential to every member of the community.
Compared to other drugs of similar nature, even the slightest dose of this micronized killer can end a life. What might be scarier is the fact that the drug is available over the counter, as a prescription drug used to treat severe pain and post-surgery discomfort, and more dangerously, through illegal markets – hidden in eye drops and nasal sprays and cut and sold under the name of other opioids on the street.
Smallwood observed this exact method of obtaining the drug during his time as a deputy.
“Several people had pill stamps,” Smallwood said. “And they were making their own pills, so they would sell these pills, and they would say ‘this is morphine’ or ‘this is Lortab.’ These pills had fentanyl in them. I’ve had addicts that I spoke to, and I’ve had numerous overdose deaths where I’ve tried to tell them the pills that you’re getting, I can tell you right now I know what they’re laced with.”
As the opiate binds to the receptors controlling pain and emotions in the brain, the numbing effects of the drug will leave the user in a state of euphoria – a high. But as they continue to chase that same feeling, they build a tolerance to the dose, meaning the only way to feel a sensation once again is to take more and more. They are hooked. The high is the only thing that brings them any relief and happiness; shortly after, their body reaches a saturation point, no longer able to handle the drug, and they overdose.
“The biggest adverse effect is something called respiratory depression,” Dr. Stephen McBride of Johnson Co. Memorial’s emergency care department said. “[Fentanyl] affects a part of the brain that regulates how quick you breathe. For instance, you are probably not consciously thinking of how quick you are supposed to be breathing. That kind of happens on autopilot. So fentanyl affects that part of the brain and stops your body from realizing that you need to take a breath. A normal person can breathe around twelve times per minute, sometimes more, sometimes less, but if you start breathing around three times per minute or one time per minute or zero times per minute, that can be very bad.”
Teenagers and their vulnerabilities to opioids
In the eyes of Smallwood, teenagers may be especially vulnerable to the dangers of opioids due to a plethora of reasons.
“It’s an easy pass off,” Smallwood said. “It’s an easy thing to hide. No odor. You can hide the pill anywhere.”
But where are students coming into contact with these opioids?
Most teenagers don’t have access to the street merchants of the inner cities nor connections to back alley producers labeling their fentanyl-cut tablets with government stamps. The answer, metaphorically and literally, is right in front of them, which makes the prospect of a fentanyl addiction all the more tangible – and more terrifyingly available – to young individuals.
“I think the main source is probably parents,” Smallwood said. “We get older. Our bodies hurt, and we get pills prescribed to us. You find out what we have, you find out the effects, and you go to your parents medicine cabinet, or your friend tells you ‘hey, my parents have this.’ And then, eventually, you can make up a fake injury and get it prescribed to yourself.”
Addiction can even come from certain factors out of the control of the user. In some cases, exposure to painkillers, whether it be from childhood surgeries, sports injuries, or other kinds of recovery, can have lasting effects on the brain chemistry of a person, making them more prone to developing a reliance on opioids later in life.
Such is the case with Leland “Alex” Plew, a Center Grove graduate and soccer player, who was hooked on opioids at a very young age due to a head surgery he received as an infant. Later, he was put back on prescription opioids to cope with the removal of his wisdom teeth and his tonsils. Tragically, Alex would overdose on heroin in his early twenties.
“By the time he was, probably, sixteen years old, he had been exposed to opioids three different times in his life through medical processes,” David Plew, Alex’s father, said.
Whether a potential user gets hooked over-the-counter, or from a dealer on the street, or by scavenging through their parent’s medicine cabinet, or even by early exposure altering the chemical signaling of their brains, the data is clear, and as the United States become more removed from the stressful and cramped era of COVID-19 – a time in which the opioid epidemic revealed its nasty jaws in full force, trends involving the crisis only continued to climb to more frightening levels.
Overprescription of opioids kicked into a higher gear than ever recorded in 1999, and preventable deaths began a strict ascent, particularly targeting older generations like the Baby Boomers as they aged and their bodies began to break down. Numbers of preventable deaths only continued to rise, beginning to affect younger generations. According to the National Safety Council, deaths increased by 41% in 2020, a repercussion that can be attributed to the COVID-19 pandemic, and they jumped another 18% in 2021. Most deaths happen to be males, but the female death rate from opioids has increased at a greater rate than males since 1999.
Overdose rates are only going up, and the problem doesn’t seem to be slowing down. According to the Indiana State Department of Health, in 2022, there were 49 opioid-related deaths in Johnson Co., comprising the majority of drug-related deaths. In March of this year, Franklin police seized 500 fentanyl pills from a local home.
How to avoid opioid addiction
The fentanyl crisis seems to be divided into three classes of people: those on the outside looking in, those who are considering experimentation with the drug and those actively using the drug.
Officer Jason Wienhorst, a narcotics officer in Johnson County, offered words of advice for students in Center Grove concerning how to avoid this drug.
“When it comes to fentanyl and opiates, it is the Russian roulette in the drug world, and you have to be very careful as to what is being presented to you as a pill, or a piece of candy even,” Wienhorst said. “The drug dealers are getting smarter and lacing a lot of different things with fentanyl, and it is because they want the high to be greater than what you got the first time, so you will keep coming back to them. If there is one thing I can say, it is to be educated of the problems with this drug and what it is doing to our society and doing to the youth of our communities.”
If someone knows a friend who is getting involved with fentanyl, the best course of action is to intervene. After all, that action could save a life.
“Talk to them,” Smallwood said. “Everyone needs someone to talk to. There is nothing wrong with asking why. That three letter word is a big question. Just letting them voice everything out can get them off of it.”
For someone pondering experimentation, the approach lacks nuance, but it is the simplest way to preserve one’s life – say no.
“It’s hard to say no,” Smallwood said. “No one wants to be the downer at a party, but you’re not the downer. You are doing so much more for yourself than what you think, and other people can see you say no. That gives hope to other people, so they don’t feel the peer pressure to do something that could harm them.”
And finally, if someone is currently taking fentanyl or an opioid of similar nature, they have to first admit to their problem.
“You have got to come to the conclusion that you have a problem,” Smallwood said. “If you don’t come to that conclusion, it is hard for you to swallow your pride and say there is something wrong here. They need to reach out, and there is nothing wrong saying you have a problem.”
More information
This is a developing story; the following is a link to a Google Form where one can share their own personal experience or the experience of another in their life if they choose to do so:
Link to Google Form: https://docs.google.com/forms/d/e/1FAIpQLSe3mCQivZBWOLUVTOKfBJdpqWfddWOqQl4kO_JpmrTqXD5XgA/viewform?usp=pp_url
Your donation will support the student journalists of Center Grove High School. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.

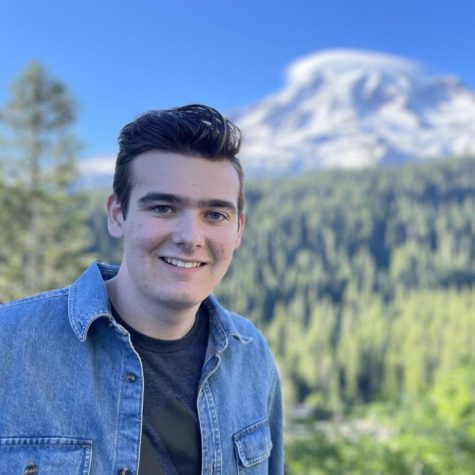
Senior Charlie LaRocca has been a staff member for two years. He started his career in publications writing sports articles and doing work for the Trojaneer...
Senior Jack Forrest is in his fourth year on staff. He started his Publications career by writing feature stories for the yearbook, as well as for the...

Senior Finn Nowacki is in his third year on staff. He started his Publications career sophomore year by mainly writing feature stories for the Trojaneer...

Senior Gourav Pany has been on staff for four years. He started his Publications career in his freshman year when writing stories about fantasy football...










Debbie Nolan • May 18, 2023 at 2:01 pm
Thank you for covering this topic! Your team did a wonderful job. Alex and Sam were both former students. Sam was in my class the year he died. I received a phone call from an assistant principal on Mother’s Day to tell me the news. It’s horrible to lose teenagers, especially when it is preventable.